Vocal Cord Dysfunction (VCD) is a chronic medical condition characterized by the vocal cords closing instead of opening during the normal breathing cycle. This unusual behavior results in breathing difficulties, coughing, and a sensation of tightness in the throat. VCD is frequently mistaken for asthma or other respiratory disorders, underlining the need to recognize its distinct symptoms. Today, we delve into the telltale signs of VCD, the diagnostic process, and effective treatment plans.
What is Vocal Cord Dysfunction (VCD)? Demystifying the Mystery
Identifying the Signs of VCD
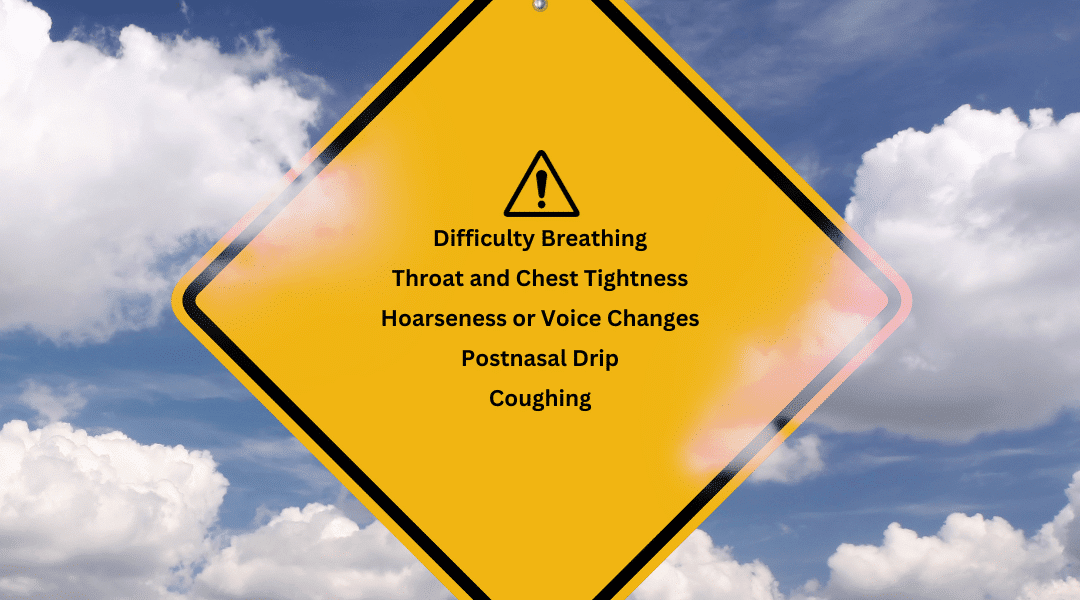
VCD presents various symptoms, including:
- Breathing Difficulties: Also known as dyspnea, challenges in breathing serve as a prominent indicator of VCD. You might experience breathlessness or an inability to regain your breath, commonly triggered by physical exertion, emotional stress, comorbid conditions, or exposure to irritants.
- Throat and Chest Tightness: With VCD, the vocal cords close during inhalation, necessitating increased effort to breathe. This can lead to a sensation of chest constriction, often attributed to inflammation around the neck and the use of accessory respiratory muscles. This tightness can also be related to Laryngopharyngeal Reflux (LPR), where stomach contents flow back into the throat, causing irritation and a sensation of discomfort.
-
Coughing: This reflexive action is instigated by the closure of vocal cords during inhalation. It acts as a protective mechanism to clear the airway of potential irritants, with the brain signaling chest and abdominal muscles to contract forcefully, followed by a rapid intake of breath and the vocal cords opening to allow air to be expelled. However, in VCD, this process can be frequently or chronically triggered due to the abnormal behavior of the vocal cords.
-
Voice Changes or Dysphonia: If you have VCD, abnormal movement of the vocal cords during speech might result in dysphonia, a condition where your voice becomes hoarse, raspy, or undergoes changes in volume, pitch, or quality. This symptom can serve as a telltale sign of Vocal Cord Dysfunction.
-
Postnasal Drip: The drainage of excess mucus from the nasal passages to the back of the throat can provoke frequent throat clearing. This can further irritate and inflame the nasal passages and vocal cords, exacerbating VCD symptoms.
How is VCD Diagnosed?
For a precise diagnosis of Vocal Cord Dysfunction, it is advisable to seek consultation with an Otolaryngologist. These medical specialists focus on disorders pertaining to the ear, nose, and throat. An Otolaryngologist conducts a procedure called a laryngoscopy, which involves the insertion of a scope equipped with a camera through the mouth or nose. This allows the physician to monitor the movement of the vocal cords in real-time, offering invaluable information regarding any abnormalities.
An Allergist-Immunologist might suspect Vocal Cord Dysfunction if symptoms such as shortness of breath are coupled with suspected allergies or environmental triggers. They conduct allergy testing to pinpoint potential allergens that could be exacerbating symptoms. Nonetheless, for a thorough examination and management of VCD, they typically recommend patients to an Otolaryngologist.
When evaluating symptoms and eliminating other potential respiratory disorders, a Pulmonologist might identify Vocal Cord Dysfunction as a possible cause. Similar to an Allergist-Immunologist, a Pulmonologist, after conducting an initial assessment, usually recommends patients to an Otolaryngologist for a more comprehensive analysis. This additional step in the diagnostic process aids in understanding the complex dynamics between the respiratory system and VCD, ensuring the most accurate diagnosis and effective treatment plan.

Effective Methods To Control VCD Symptoms
Upon diagnosing VCD, an Otolaryngologist works in conjunction with patients to formulate an appropriate management strategy. The array of options available to control VCD symptoms comprises:
- Speech Therapy: Under the guidance of a speech-language pathologist, patients with VCD can learn methods to regulate their vocal cord movement and enhance breathing patterns.
- Evasion of Triggers: Recognizing and steering clear of triggers plays a crucial role in controlling VCD symptoms.
- Medicinal Treatments: Medications such as anti-inflammatories, antihistamines, inhaled corticosteroids, or benzodiazepines like Ativan might be prescribed to keep symptoms in check.
- Psychological Assistance: As stress and anxiety can intensify VCD symptoms, engaging in counseling or therapeutic sessions could prove beneficial.
- Education and Personal Care: Gaining comprehensive knowledge about VCD and the ability to identify early signs of an episode can empower individuals to manage their symptoms effectively.
FAQs Section
Frequently Asked Questions about Vocal Cord Dysfunction (VCD)
Can VCD be cured? At present, we don’t have a complete cure for VCD. However, it’s quite feasible to manage this condition effectively using appropriate treatments, strategies, and wellness plans. The objective of these interventions is to mitigate symptoms and enhance your daily living experience.
How does VCD affect daily life? The effects of VCD on day-to-day living can range widely, contingent on symptom intensity. It can impede routine physical activities like exercising or doing household chores due to breathing challenges. In more severe situations, it can incite anxiety stemming from the fear of VCD episodes. Nevertheless, with a well-tailored therapeutic approach and appropriate self-care practices, individuals battling VCD can still lead enriching and satisfying lives.
Can VCD be prevented? While we don’t have a failsafe method to completely ward off VCD, you can substantially reduce the likelihood of experiencing episodes by steering clear of known triggers and maintaining a robust overall health condition.
How is VCD different from asthma? While VCD and asthma exhibit common symptoms, notably difficulties in breathing, they represent distinct conditions. Asthma primarily impacts the exhalation process and pertains to the lungs, whereas VCD influences the inhalation process and pertains to the throat region. Additionally, asthma typically responds favorably to inhalers and other asthmatic drugs, which generally prove to be ineffective for treating VCD.
Can children get VCD? Indeed, VCD can impact individuals across all age groups, encompassing even children. If you notice symptoms such as difficulties in breathing or voice alterations in your child, it’s recommended to seek advice from a pediatrician or a pediatric Otolaryngologist.
How can Breathe Body Wellness help me manage my VCD? At Breathe Body Wellness, we leverage the expertise of a Board-Certified Nurse Coach who will guide you through your VCD journey. Our approach integrates breathwork, physical exercise, and personalized meditation techniques to manage VCD symptoms effectively. To discuss these methods and shape a program tailored to your unique needs, we extend an invitation for a no-obligation consultation.
Bear in mind that handling VCD effectively requires adaptability, perseverance, and a deep understanding of the condition. By adopting effective strategies and crucial lifestyle modifications, you can gain control and significantly improve your holistic wellness. Are you ready to take the reins and enhance your life quality? We invite you to share your VCD experience in the comments below, offering invaluable insights and support to others encountering similar hurdles. Always remember, you’re not isolated in this journey.

